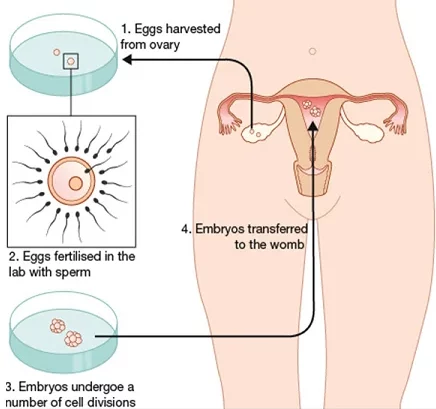
Embryo transfer stands as the pivotal and culminating step in the intricate journey of in vitro fertilization (IVF), representing the gateway to the realization of a successful pregnancy. This transformative procedure, typically undertaken 3 to 5 days post-fertilization, plays a paramount role in determining the ultimate outcome of the IVF process. Administered under mild sedation or local anesthesia, the transfer is designed to be a relatively simple and painless experience.
Preparing for Embryo Transfer:
The groundwork for a successful transfer begins with a meticulous assessment of the woman’s uterus. This pre-transfer evaluation ensures an environment conducive to implantation. Utilizing ultrasound technology, the thickness and pattern of the endometrial lining are scrutinized, and hormone levels are evaluated. Any necessary adjustments to the woman’s medication regimen are made to optimize conditions for successful implantation.
The Embryo Transfer Procedure:
Conducted by a skilled reproductive endocrinologist or fertility specialist, embryo transfer is a delicately orchestrated process. The selected high-quality embryo(s) are gently loaded into a thin, flexible catheter. Employing ultrasound guidance to guarantee precision, the catheter is then carefully inserted through the cervix and into the uterus. Upon achieving the optimal position, the embryos are released into the uterine cavity with precision. Subsequently, the catheter is removed, and the woman is advised to rest briefly, fostering a conducive post-transfer environment.
Factors Influencing the Success of Embryo Transfer:
The success of the transfer hinges on a confluence of factors. Embryo quality, marked by regular cell division and minimal fragmentation, is a pivotal determinant. Equally influential are endometrial receptivity and the woman’s age, with younger individuals generally experiencing heightened success rates due to a surplus of healthy eggs and embryos.
Single vs. Multiple Embryo Transfer:
Evolving from historical practices of multiple embryo transfers, contemporary approaches advocate for elective single embryo transfer (eSET). This strategic shift seeks to balance success rates while mitigating the heightened risks associated with multiple pregnancies, fostering a safer environment for both the mother and potential offspring.
After Embryo Transfer:
Post-transfer care is paramount, with women advised to take a few days of respite, abstaining from strenuous activities and heavy lifting. Progesterone supplementation is commonly prescribed to fortify the uterine lining, augmenting the chances of successful implantation. Approximately two weeks post-transfer, a blood test measuring human chorionic gonadotropin (hCG) is administered. Elevated hCG levels confirm successful implantation and herald the initiation of pregnancy.
Implantation Failure and Next Steps:
Despite the meticulous efforts of fertility specialists, not every embryo transfer culminates in a successful pregnancy. Implantation failure may be attributed to factors such as poor embryo quality, inadequate endometrial receptivity, chromosomal abnormalities, or immunological factors. In the event of an unsuccessful initial transfer, diverse options for subsequent IVF cycles are considered.
In cases where additional embryos were cryopreserved during the initial IVF cycle, the avenue of frozen embryo transfer (FET) is explored. This less invasive and cost-effective approach bypasses the need for ovarian stimulation and egg retrieval. Alternatively, in scenarios where no viable embryos from the initial cycle are available, couples may embark on another complete IVF cycle. Such instances may involve adjustments to the treatment protocol, such as medication changes, preimplantation genetic testing (PGT), or the exploration of alternative treatment options like donor eggs, sperm, or surrogacy.
Embryo transfer undeniably stands as a linchpin in the IVF process, wielding substantial influence over treatment outcomes. While success is contingent on a myriad of factors, including embryo quality, endometrial receptivity, and patient age, ongoing advancements in assisted reproductive technology and personalized treatment protocols kindle hope for couples navigating the intricate terrain of infertility. These innovations empower individuals to persevere in their pursuit of the dream of building a family, making the possibilities inherent in IVF even more promising.