Infertility Treatments – Endometriosis
The Endometrium
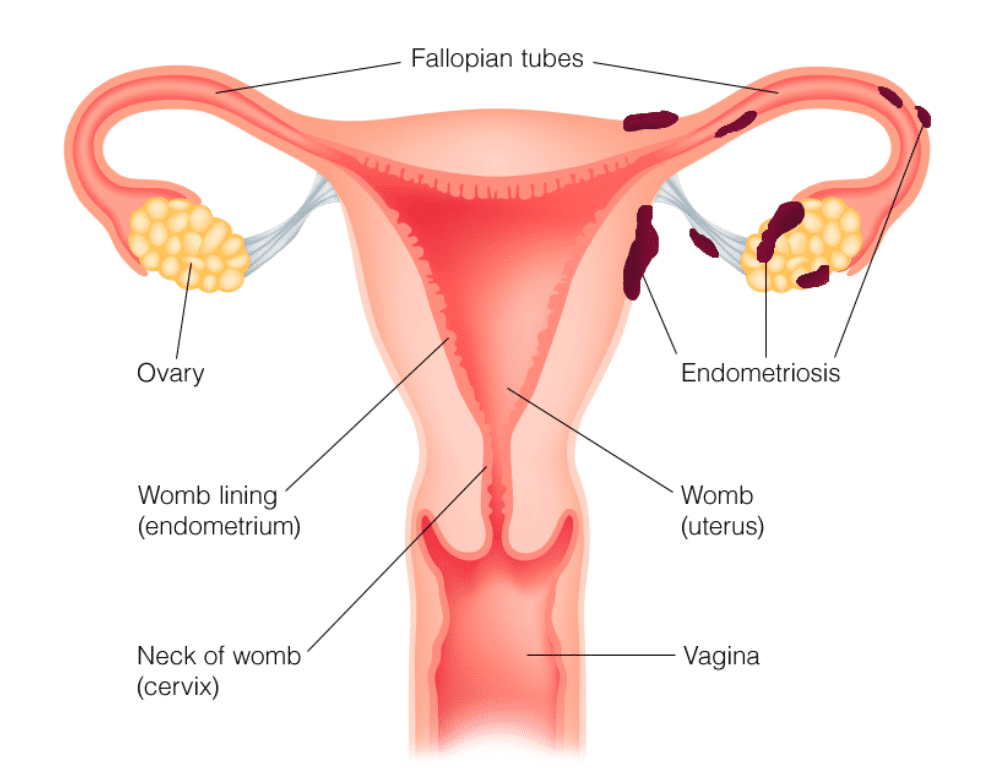
The endometrium is the inner lining of the uterus, a crucial component of the female reproductive system. Undergoing cyclic changes in response to hormonal fluctuations throughout the menstrual cycle, the endometrium thickens and becomes more vascular, preparing a suitable environment for the potential implantation of a fertilized egg. If fertilization does not occur, the endometrial lining is shed during menstruation. The dynamic nature of the endometrium, regulated by hormones like estrogen and progesterone, reflects its pivotal role in supporting embryonic development and maintaining reproductive health.
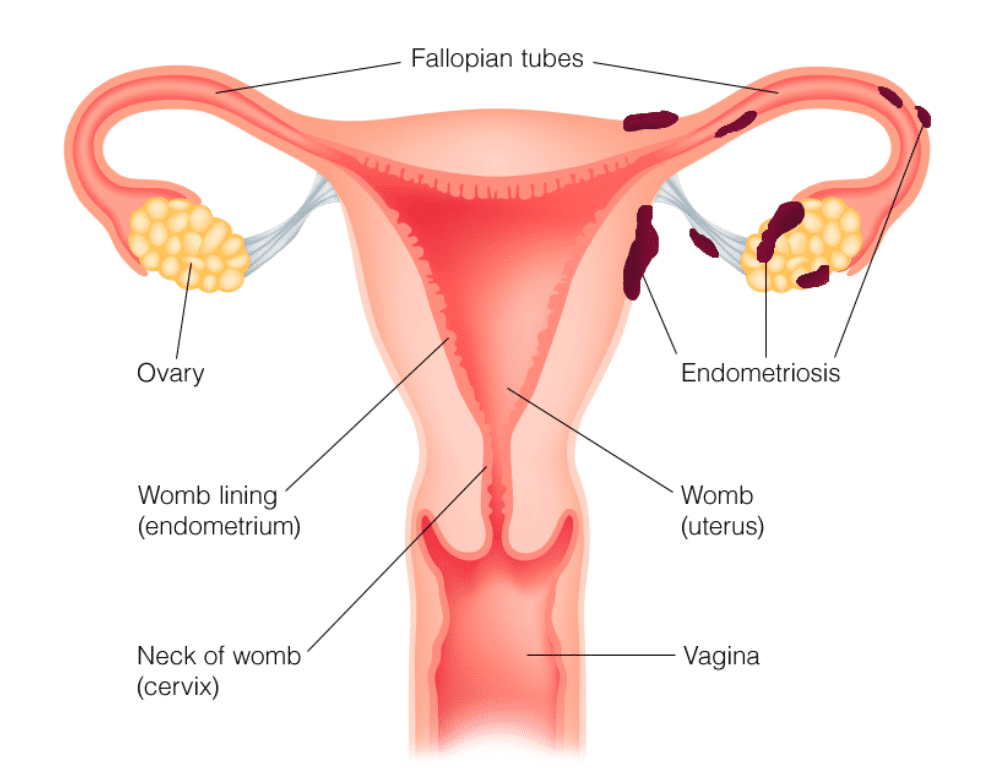
What Is Endometriosis?
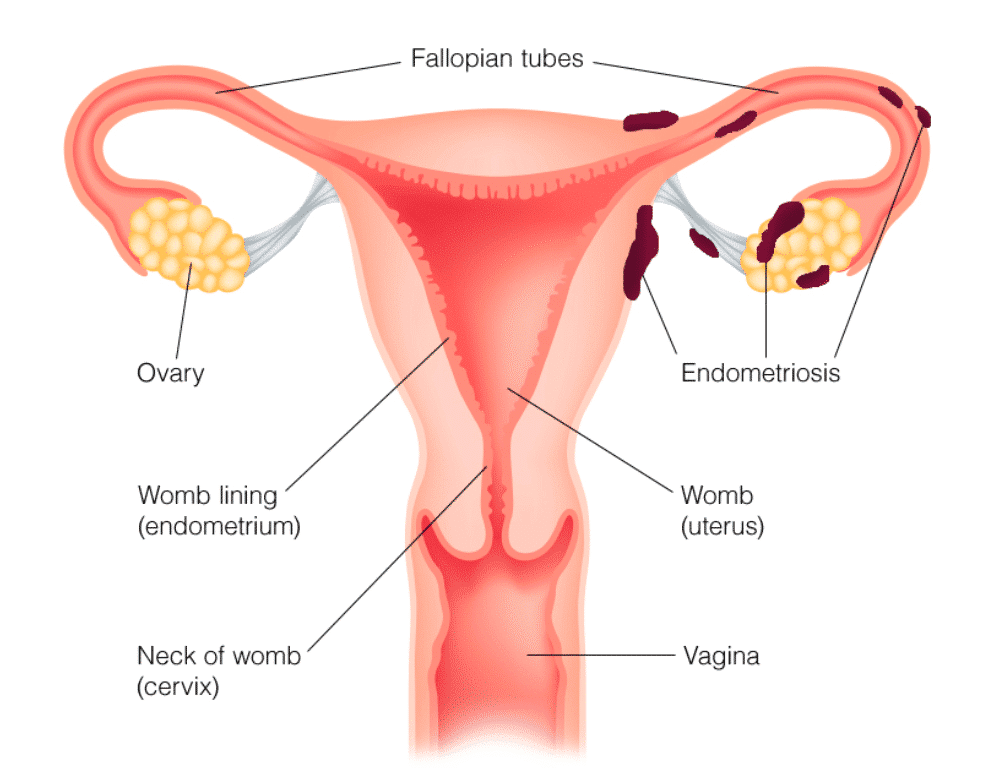
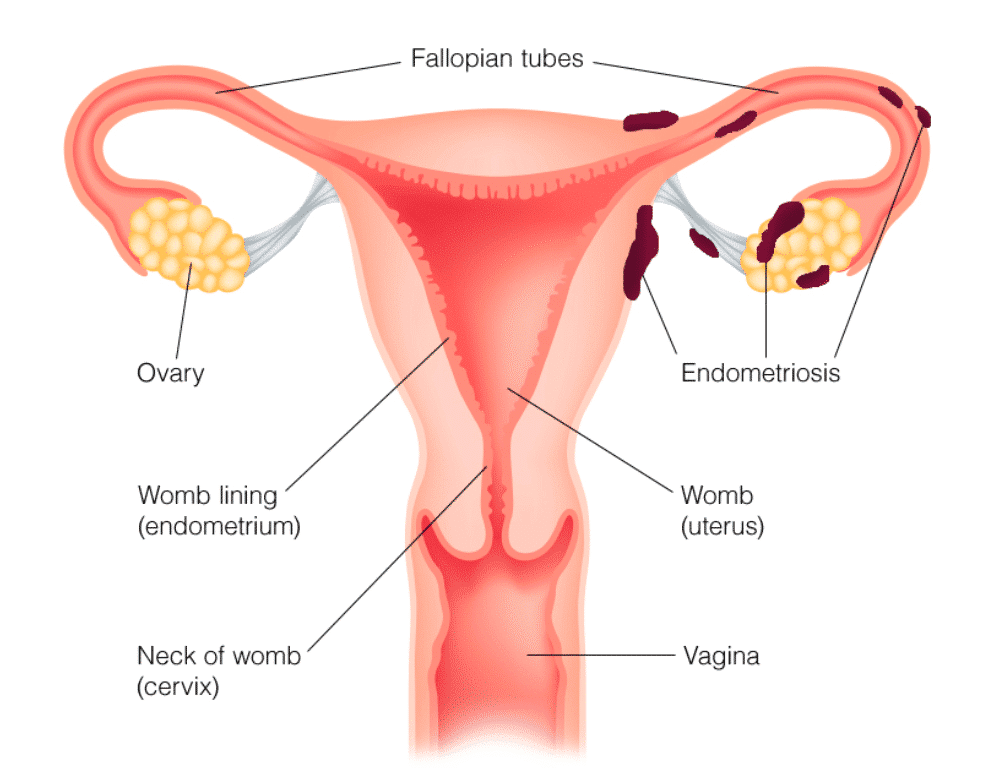
Endometrial tissue may attach to organs in the pelvis or to the peritoneum. It also may be found in other parts of the body. This is very rare, though. Endometrial tissue that grows in the ovaries may cause a cyst (also known as an endometrioma) to form.
Endometrial tissue outside the uterus responds to change in hormones. It also breaks down and bleeds like the lining of the uterus during the menstrual cycle. This bleeding can cause pain, especially before and during your period.
The breakdown and bleeding of this tissue each month also can cause scar tissue, called adhesions. Sometimes adhesions bind organs together. Adhesions also can cause pain.
The symptoms of the endometriosis often worsen over time. In many cases, treatment may help keep the condition from getting worse.
Who Is at Risk?
Endometriosis can affect women of any age during their reproductive years, typically starting in adolescence and continuing until menopause. However, several factors may increase the risk of developing endometriosis:
- Family History: If a woman has a close relative (mother, sister, or daughter) with endometriosis, her risk of developing the condition may be higher.
- Menstrual History: Short menstrual cycles (less than 27 days) or long periods of menstruation (more than seven days) may be associated with an increased risk of endometriosis.
- Obstruction of Menstrual Flow: Anything that impedes the normal flow of menstrual blood, such as a blockage or backward flow of menstrual fluid, may increase the likelihood of endometriosis.
- Delayed Childbearing or Never Having Children: Women who delay childbirth or remain childless may have a higher risk of developing endometriosis.
- Abnormalities in the Reproductive Tract: Structural issues that affect the normal passage of menstrual flow or the ability of the uterus to contract and expel menstrual tissue may contribute to endometriosis.
- Autoimmune Diseases: Some autoimmune conditions have been associated with an increased risk of endometriosis.
It’s important to note that while these factors may increase the risk, they don’t guarantee the development of endometriosis, and the condition can still occur in the absence of these factors. Conversely, some women with multiple risk factors may never develop endometriosis. The exact cause of endometriosis remains unclear, and more research is needed to fully understand its origins and contributing factors. If someone suspects they have endometriosis due to symptoms such as pelvic pain or fertility issues, it’s essential to consult with a healthcare professional for an accurate diagnosis and appropriate management.
Symptoms
Endometriosis symptoms can vary widely among individuals, and some women with the condition may experience mild symptoms or none at all. Common signs and symptoms of endometriosis include:
- Pelvic Pain: This is a hallmark symptom of endometriosis. The pain can vary and may include:
- Painful menstrual cramps that may worsen over time.
- Chronic pelvic pain outside of menstruation.
- Pain during or after sexual intercourse.
- Menstrual Irregularities: Women with endometriosis may experience changes in their menstrual cycle, including:
- Heavy menstrual bleeding.
- Irregular periods.
- Painful periods (dysmenorrhea).
- Painful Bowel Movements or Urination: Endometriosis can cause pain during bowel movements or urination, especially during menstruation.
- Painful Ovulation: Some women with endometriosis may experience pain during ovulation.
- Painful Pelvic Exams: Pelvic examinations or intercourse may be painful for women with endometriosis.
- Infertility: Endometriosis is sometimes associated with fertility issues. The condition can lead to the formation of adhesions and scar tissue, which may interfere with the normal functioning of the reproductive organs.
It’s important to note that the severity of symptoms doesn’t necessarily correlate with the extent or stage of endometriosis. Some women with mild cases may experience significant pain, while others with severe endometriosis may have minimal discomfort.
Diagnosis
The diagnosis of endometriosis typically involves a combination of medical history, physical examinations, and sometimes imaging studies or surgical procedures. Here is an overview of the diagnostic process:
- Medical History and Symptom Evaluation: The healthcare provider will start by gathering a detailed medical history, including information about the nature, duration, and severity of symptoms. Common symptoms include pelvic pain, painful menstruation, and potential fertility issues.
- Pelvic Examination: A pelvic examination may be performed to check for any abnormalities, tenderness, or masses in the pelvic region. However, it’s important to note that endometriosis cannot be definitively diagnosed through a pelvic exam alone.
- Imaging Studies: While imaging studies such as ultrasound or magnetic resonance imaging (MRI) can help visualize the pelvic organs and detect abnormalities, they are not conclusive for diagnosing endometriosis. However, these tests may be used to rule out other conditions or identify cysts associated with endometriosis (endometriomas).
- Laparoscopy: The most definitive method for diagnosing endometriosis is through a surgical procedure called laparoscopy. During laparoscopy, a thin, lighted tube with a camera (laparoscope) is inserted through small incisions in the abdomen. This allows the healthcare provider to directly visualize and confirm the presence of endometrial tissue outside the uterus. If endometriosis is identified, the surgeon may also perform therapeutic procedures, such as removing or treating the abnormal tissue.
- Biopsy: In some cases, a biopsy may be taken during laparoscopy to confirm the presence of endometrial tissue and rule out other conditions.
It’s important to emphasize that laparoscopy is often reserved for cases where there is a strong suspicion of endometriosis or when conservative treatments have not provided relief. The decision to undergo laparoscopy is usually made collaboratively between the healthcare provider and the patient.
If a woman suspects she has endometriosis based on symptoms, she should consult with a healthcare professional. Early diagnosis and intervention can help manage symptoms and potentially address fertility concerns associated with endometriosis.
Treatment
The treatment of endometriosis aims to manage symptoms, alleviate pain, and improve overall quality of life. The specific approach to treatment depends on factors such as the severity of symptoms, the desire for fertility, and the individual’s overall health. Treatment options for endometriosis include:
- Pain Medications: Over-the-counter pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can help manage the pain associated with endometriosis. In more severe cases, prescription pain medications may be recommended.
- Hormonal Therapies: Hormonal treatments aim to suppress or regulate the menstrual cycle to reduce the growth and activity of endometrial tissue. Common hormonal therapies include:
- Birth Control Pills: Oral contraceptives can help regulate the menstrual cycle and reduce the severity of symptoms.
- Progestin Therapy: Progestin, in various forms such as pills, injections, or intrauterine devices (IUDs), can help control the growth of endometrial tissue.
- Gonadotropin-Releasing Hormone (GnRH) Agonists and Antagonists: These medications temporarily induce a menopausal state, suppressing estrogen production and slowing the growth of endometrial tissue. They are often used for short-term symptom relief.
- Surgery: In cases where symptoms are severe or fertility is a concern, surgical intervention may be recommended. The most common surgical procedure for endometriosis is laparoscopy, during which the surgeon can remove or ablate (destroy) endometrial tissue. In more extensive cases, a more invasive procedure called laparotomy may be necessary.
- Hysterectomy: In severe cases, when other treatments have not been effective and the patient does not desire future pregnancy, a hysterectomy (removal of the uterus) may be considered. This is usually accompanied by the removal of the ovaries (oophorectomy) if endometriosis has significantly affected them.
- Complementary Therapies: Some individuals find relief from symptoms through complementary approaches such as acupuncture, physical therapy, dietary changes, and stress management techniques. While these methods may not be a cure, they can be used as part of a comprehensive treatment plan.
It’s important for individuals with endometriosis to work closely with their healthcare providers to develop a personalized treatment plan. The choice of treatment depends on factors such as the severity of symptoms, the individual’s reproductive goals, and overall health. Regular follow-up visits are typically recommended to monitor the effectiveness of the chosen treatment and make adjustments as needed.