Understanding TESE: A Guide to Treating Male Infertility
Male infertility is a significant challenge that numerous couples face globally. Among the various causes, non-obstructive azoospermia, a condition where sperm are produced but not present in the ejaculate, stands out. Testicular Sperm Extraction (TESE) offers a ray of hope for men afflicted by this condition. This detailed guide delves into what TESE is, its procedure, and how it aids in combating male infertility.
What is Testicular Sperm Extraction (TESE)?
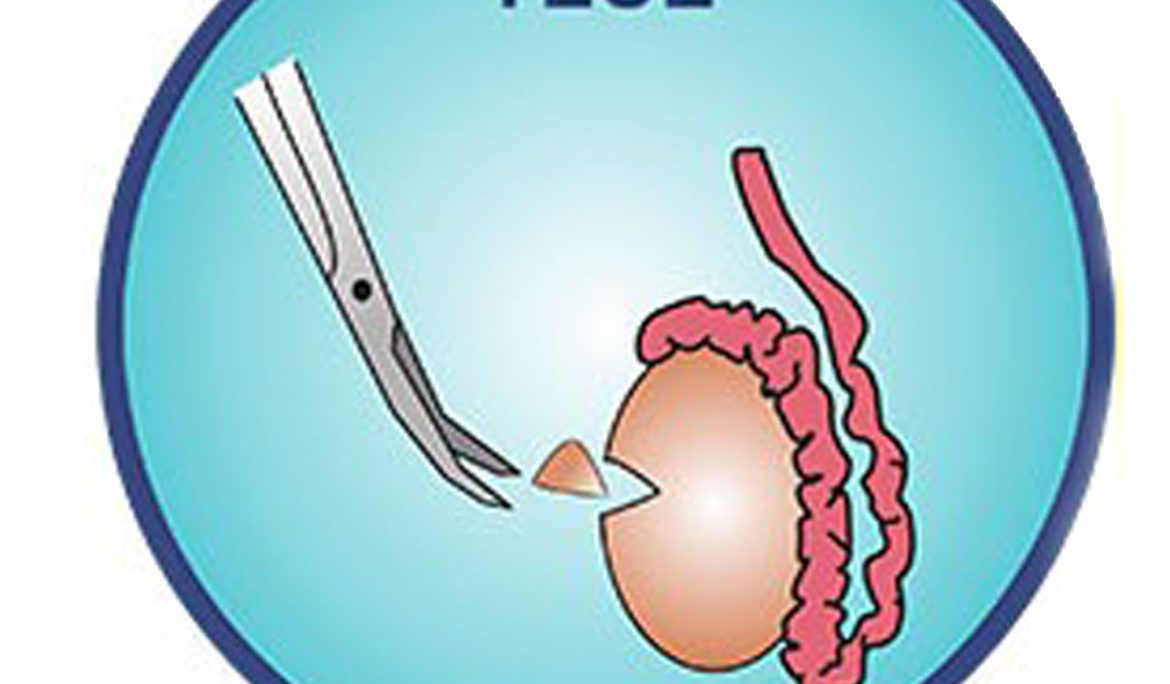
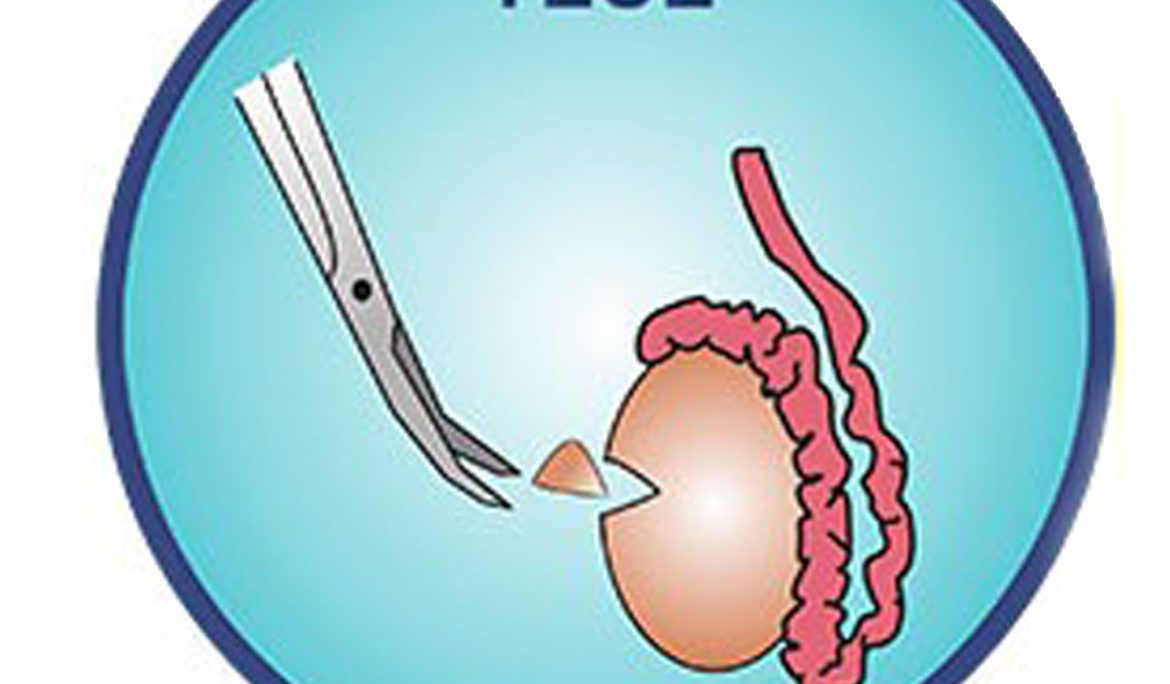
TESE is an invasive medical procedure tailored to retrieve sperm directly from the testes. This method is particularly beneficial for men who suffer from non-obstructive azoospermia. Unlike Testicular Sperm Aspiration (TESA), which involves extracting sperm using a needle, TESE involves making a small incision in the testicle to obtain tissue samples.
The TESE Procedure Explained
Performed under local or general anesthesia, the TESE procedure involves a urologist making a minor incision in the scrotum to access the testicle. The specialist then extracts small samples of testicular tissue. These samples are immediately examined by an embryologist to isolate viable sperm. The process typically lasts between 30 minutes to an hour and is often conducted on an outpatient basis.
Applications of TESE in Assisted Reproduction
The primary use of sperm retrieved through TESE is in assisted reproductive technologies (ART), notably In Vitro Fertilization (IVF) and Intracytoplasmic Sperm Injection (ICSI). In situations where the sperm count is extremely low or the sperm have poor mobility, ICSI is particularly advantageous as it requires only one sperm to be injected directly into an egg.
Advantages of TESE
TESE is an essential procedure for men who have viable sperm production within the testes but lack sperm in their ejaculate. It enables these individuals to pursue biological fatherhood, offering a lifeline to couples facing severe male infertility. Furthermore, TESE can be synchronized with the female partner’s egg retrieval process, aligning the couple’s fertility treatment timelines.
Risks and Considerations of TESE
While TESE is a breakthrough in treating male infertility, it comes with its share of risks such as postoperative pain, infection, or bleeding. Additionally, there’s no guarantee that the procedure will yield viable sperm, which may necessitate additional attempts or alternative approaches.
Who is a candidate for the TESE procedure?
Men diagnosed with non-obstructive azoospermia are ideal candidates for TESE. This includes men who have genetic conditions, hormonal imbalances or have had unsuccessful results from less invasive sperm retrieval methods.
How is TESE different from TESA?
TESE involves making a small incision in the testes to extract tissue, whereas TESA (Testicular Sperm Aspiration) uses a needle to aspirate sperm. TESE is generally considered when TESA has been unsuccessful or is deemed less likely to be effective.
Is the TESE procedure painful?
TESE is typically performed under local or general anesthesia to minimize discomfort. Post-procedure, some men may experience pain or discomfort, which can usually be managed with pain relief medication.
What are the risks associated with TESE?
Risks include bleeding, infection, and potential damage to the testicular tissue. However, these complications are rare, and the procedure is considered relatively safe.
How successful is TESE in retrieving sperm?
Success rates vary depending on the individual’s condition and the reason for azoospermia. While TESE can be effective, there’s no guarantee it will yield viable sperm for every patient.
What happens to the sperm retrieved from TESE?
Sperm extracted through TESE can be used in assisted reproductive techniques such as IVF or ICSI. If not used immediately, the sperm can be frozen for future use.
Can TESE be repeated if it doesn’t yield viable sperm the first time?
Yes, TESE can be repeated, but this depends on the individual’s circumstances and the outcomes of the first procedure. Discussing options with a fertility specialist is crucial.
How long does recovery from TESE take?
Recovery varies but typically, men can return to normal activities within a few days to a week. It’s important to follow post-operative care instructions to ensure proper healing.
How do I prepare for a TESE procedure?
Preparation might include stopping certain medications, performing blood tests, and refraining from eating or drinking before the procedure. Your healthcare provider will give specific instructions based on your situation.
What is the cost of a TESE procedure?
The cost can vary depending on the clinic, geographic location, and whether additional fertility treatments are required. Discussing cost and insurance coverage with your clinic is advisable. Fertility treatments are cheaper in Turkey.
Can TESE help in cases of obstructive azoospermia?
TESE is typically used for non-obstructive azoospermia. For obstructive azoospermia, other procedures like micro-TESE or surgical correction of the obstruction might be more appropriate.
Conclusion
TESE has revolutionized the field of reproductive medicine, offering new possibilities for couples grappling with male infertility due to non-obstructive azoospermia. It epitomizes the strides made in medical technology and techniques, empowering many to overcome intricate fertility issues. However, it’s crucial for individuals considering this procedure to thoroughly discuss the potential risks and benefits with their healthcare provider, ensuring an informed decision is made.