Varicocele, a condition characterized by the enlargement of the veins within the scrotum, is a common issue that can lead to pain, swelling, and in some cases, fertility problems in men. While several treatments are available, microsurgical varicocelectomy has emerged as a preferred option for many due to its effectiveness, safety, and minimal invasiveness. This article delves into the reasons why microsurgical varicocelectomy is often the treatment of choice for varicocele.
High Success Rates and Improved Fertility
One of the primary reasons to choose microsurgical varicocelectomy is its high success rate. Studies have shown that this procedure effectively alleviates the symptoms of varicocele, with a significant number of patients experiencing improvements in pain and discomfort. Moreover, for men facing infertility issues related to varicocele, microsurgical varicocelectomy has been linked to improvements in sperm quality and motility, thereby enhancing fertility prospects.
Minimized Risks of Complications
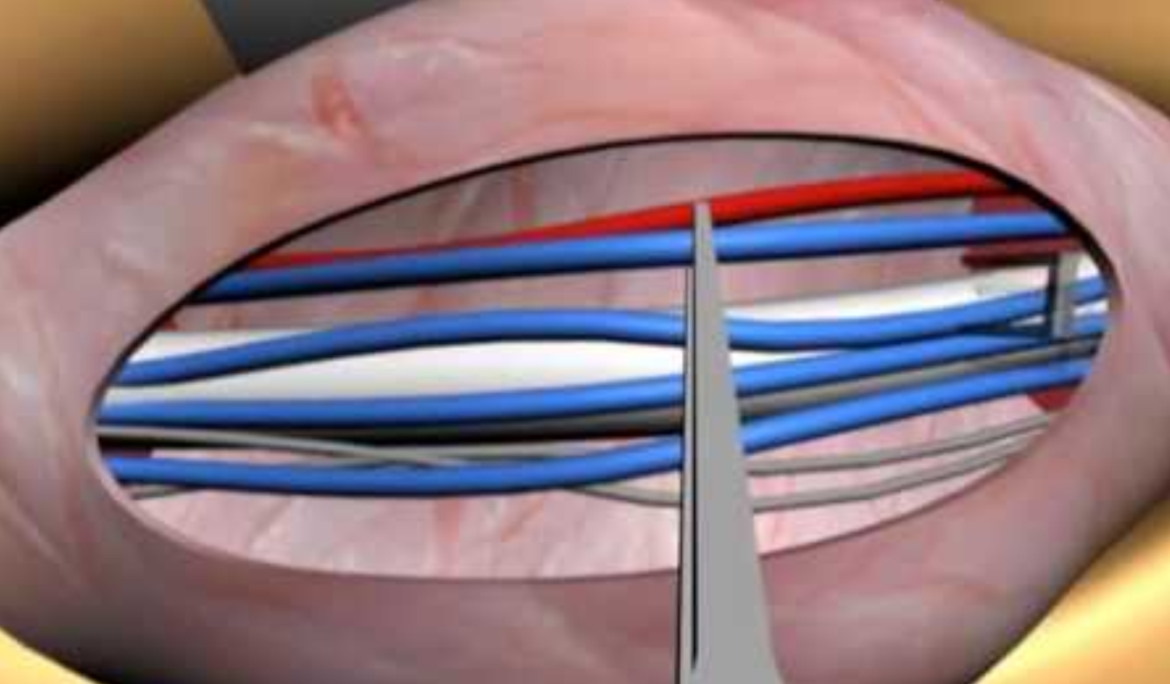
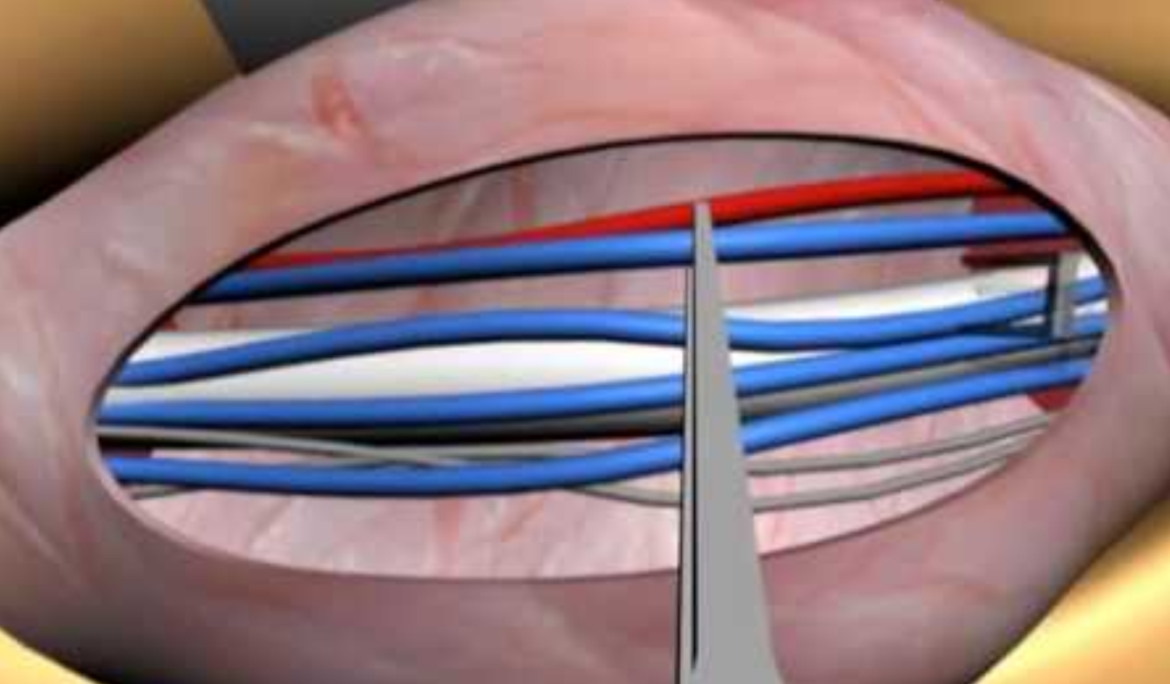
The precision of microsurgery significantly reduces the risk of complications common to other varicocele treatment methods. The use of a microscope allows surgeons to accurately identify and preserve important structures such as arteries and lymphatic vessels, thereby minimizing the chances of accidental damage. This precision reduces the risks of postoperative complications such as hydrocele (accumulation of fluid around the testicle) and recurrence of varicocele.
Reduced Pain and Quicker Recovery
Microsurgical varicocelectomy is known for its minimal invasiveness, which translates to less postoperative pain and a quicker recovery time compared to traditional surgical methods. Patients typically return to their normal activities within a few days, with many reporting minimal discomfort during the recovery period. This quick recovery is a significant advantage for those who cannot afford a lengthy downtime.
Lower Recurrence Rates
The meticulous approach of microsurgical varicocelectomy leads to lower recurrence rates of varicocele. By using the microscope to ensure that all the affected veins are identified and tied off, surgeons can effectively prevent the condition from recurring. This is a significant benefit over other treatments, where incomplete treatment of the affected veins can lead to higher chances of varicocele returning.
Improved Cosmetic Outcomes
Given the precision with which microsurgical varicocelectomy is performed, the incisions made during the procedure are typically small and result in minimal scarring. This aspect is particularly important for patients concerned about the cosmetic appearance of their scrotum post-surgery. The reduced risk of atrophy or damage to the testicular tissue further contributes to satisfactory cosmetic outcomes.
FAQs for Microsurgical Varicocelectomy
What is microsurgical varicocelectomy?
Microsurgical varicocelectomy is a surgical procedure used to treat varicocele, a condition characterized by the enlargement of veins within the scrotum. It involves the use of a surgical microscope to accurately identify and ligate (tie off) the dilated veins, minimizing damage to surrounding structures.
Who is a good candidate for microsurgical varicocelectomy?
Good candidates for microsurgical varicocelectomy include men who are experiencing symptoms from varicocele such as pain, testicular atrophy, or fertility issues. It is also recommended for those who have a varicocele that is visible or palpable.
How does microsurgical varicocelectomy improve fertility?
Microsurgical varicocelectomy can improve fertility by alleviating the adverse effects of varicocele on sperm production and quality. By correcting the abnormal blood flow, the procedure can enhance sperm concentration, motility, and overall semen parameters, potentially improving the chances of conception.
What are the risks associated with microsurgical varicocelectomy?
While microsurgical varicocelectomy is considered safe and minimally invasive, as with any surgical procedure, there are potential risks. These may include infection, hematoma, hydrocele formation, and recurrence of varicocele. However, the risk of complications is significantly lower compared to other treatment methods due to the precision of the surgical technique.
How long is the recovery period after microsurgical varicocelectomy?
The recovery period after microsurgical varicocelectomy is relatively short, with many patients able to resume normal activities within a few days. Complete recovery and the resolution of symptoms may take a few weeks, depending on the individual’s condition and the extent of the surgery.
Will there be noticeable scarring after the procedure?
Due to the minimally invasive nature of microsurgical varicocelectomy and the small incisions used, scarring is typically minimal. The incisions are usually made in the scrotal area, where scars can be less visible.
Is microsurgical varicocelectomy covered by insurance?
Coverage for microsurgical varicocelectomy varies by insurance provider and plan. It is often covered when deemed medically necessary, such as for pain relief or to address infertility issues. Patients should consult with their insurance company to understand their coverage details.
Can varicocele recur after microsurgical varicocelectomy?
While the recurrence rate of varicocele after microsurgical varicocelectomy is low, recurrence is possible. The procedure’s high success rate and the meticulous approach used significantly reduce the likelihood of recurrence compared to other treatments.
How is microsurgical varicocelectomy performed?
The procedure is performed under general anesthesia. A small incision is made in the groin or scrotum, and the surgeon uses a microscope to identify and isolate the dilated veins. These veins are then ligated, while preserving arterial and lymphatic circulation, to prevent varicocele from recurring and minimize complications.
Can I have children after microsurgical varicocelectomy?
Many men who undergo microsurgical varicocelectomy for fertility reasons see an improvement in their semen analysis results and potentially their fertility outcomes. While individual results vary, the procedure is often performed with the goal of improving a man’s ability to father children.